Asian and NHPI health equity is elusive without disaggregated data
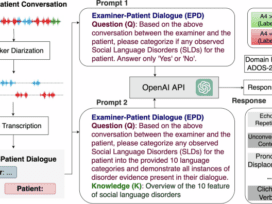
Kaiser Family Foundation health equity researchers took a deep dive into 2021 American Community Survey data to examine how demographics, health coverage and other social determinants of health drive health and healthcare for Asian…
Continue Reading